Low-Frequency Ultrasonic Debridement and Collagenic Therapy in the management of chronic leg ulcers with a new integrated method
The present Practice Statement regards the management of chronic leg ulcers using a New Integrated Method based on the use of Low Frequency Ultrasonic Debridement (LFUD) combined with a Collagenic Therapy. 312 leg ulcers in 286 patients were treated with LFUD (Genera UDD - Italia Medica, Italy) and with a device for a Collagenic Infusion Therapy (Genix-IT - Italia Medica, Italy). Genix – IT is a collagen device derived from heterologous pericardium and peritoneum in the form of dried, sterile and resorbable membrane, of 300 - 400 μm thick, with stimulation capabilities of granulation. The membrane is supported by a catheter for infusion of drugs for bacterial killing and pain control. Completed the connectival regeneration, a Epitelial Growth Inducer (Genix EGI ), in the form of sterile collagen membrane, 200-250 μm thick, was made to adhere to the edges of the lesion to allow the re-epithelialization. The healed lesions were 307, while 4 in the terminal phase of healing; 1 is not healed in a patient treated with immunosuppressive anti-VEGF; healing times varies between 3 and 15 months. Ultrasonic debridement combined with Genix technology helps to effectively solve regeneration problems and to control infections and pain of leg ulcers.
Debridement is the first step necessary to allow the initiation of the granulation process through the removal of barriers that impair wound healing. Ultrasound can be considered one of the most effective methods of wound debridement, differing from the others by its specific physical characteristics of application, highly favorable to the healing process. LFUD is less aggressive than other methods and more selective in the removal of devitalized tissues that are not cut but have undergone a detachment, fragmentation and emulsification preserving healthy tissue. Antimicrobial activity of ultrasound has been demonstrated and widely recognized1,2,3, while other debridement techniques have not proved equally effective in reducing the bacterial load of wounds4,5,6. Although the debridement is essential to promote wound healing7, it represents only the first stage of therapeutic treatment. The removal of devitalized materials, often infected, is not able on its own to ensure a rapid trigger of the granulation process until the final healing. Despite the debridement of the wounds, their chronicity persists due to several altered physiologies at the cellular level8. Chronic ulcers present a high number of neutrophils and macrophages that produce large amounts of inflammatory mediators and proteolytic enzymes. The inflammatory mediators stimulate endothelial cells to produce exudate, high levels of proteases, especially matrix metalloproteases, cause tissue degradation and inhibition of the formation of a functional extracellular matrix (ECM) essential for healing9,10. The chronic ulcers frequently have bacterial colonization, a state of chronic inflammation, degradation of ECM with a preponderance of senescent fibroblasts and degraded and inactive growth factors. Debridement may need to be repeated and various types of dressings to be proposed in the post debridement to rebalance the cellular activity and accelerate the rate of new tissue formation. Topically placed collagen has been proven to possess qualities in reducing excessive levels of protease, reestablishing balance in wound environment and promoting wound healing by activating inflammatory cells and neoangiogenesis11. Research has demonstrated that Tipe I collagen matrices induces fibroblast and keratinocyte migration, essential to the formation of granulation tissue and final re-epithelialization of the wound12,13. LFUD combined with collagen therapy, integrated in a New Method, is the subject of our study about the treatment of chronic ulcers of the lower limbs.
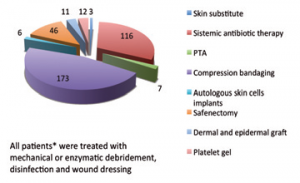 Table 1. Previous care performed by patients in other centers without success over a period time ranging between 3 months to 5 years. *Same patients have undergone several types of treatements listed above.
Table 1. Previous care performed by patients in other centers without success over a period time ranging between 3 months to 5 years. *Same patients have undergone several types of treatements listed above.312 chronic leg ulcers in 286 patients were treated. These patients received previous treatments for this pathology at other centers over a period of time ranging between 3 months to 5 years without success. 252 treated leg ulcers presented a prevalence of chronic venous insufficiency, 25 were of mixed types; 21 caused by vasculitis; 6 were hypertensive ulcers and 8 were traumatic. 146 ulcers resulted clinically infected according to the principles of best practice14. The size of the ulcers was between 5 square centimeters and 320 square centimeters. Previous treatments, listed in Table 1, have always provided mechanical or enzymatic debridement, disinfection and wound dressing; antibiotic therapy was always systemic.
LOW-FREQUENCY ULTRASONIC DEBRIDEMENT
 Figure 1. Sonic probe ultrasonically activated and irrigated with saline solution. The presence of plastic cover put on the tip avoid dispersion of nebulization during debridement.
Figure 1. Sonic probe ultrasonically activated and irrigated with saline solution. The presence of plastic cover put on the tip avoid dispersion of nebulization during debridement.Wound bed preparation carried out in all 312 chronic leg ulcers using LFUD with Genera UDD (Italia Medica, Italy) which is an ultrasonic debrider composed of an ultrasound generator operating in continous mode with the activation of a steel probe mounted on a piezoelectric transducer and vibrating at a frequency of 26 KHz. In order to perform the debridement of cutaneous ulcers various types of interchangeable sonic probes were used for dissection of necrosis or emulsification of fibrinous and devitalized tissues. It resulted in removal of altered material, even the one strongly adherent to the ulcer bed. These probes have a working part that acts in contact with the tissues with transverse vibrations of 30 μm amplitude, peak to peak. The working part is irrigated with saline solution under pressure using a peristaltic pump and a plastic cover can be put on the tips to avoid dispersion of nebulization preserving air and space contamination (Figure 1). A topical analgesic therapy with 2% lidocaine before ultrasonic debridement was performed in the majority of cases, using very low doses which on average were about 5ml, not surpassing 15ml of anesthetic even in extended ulcers.
COLLAGENIC INFUSION THERAPY
 Figure 2. At the end of an ultrasonic debridement of a phlebostatic ulcer.
Figure 2. At the end of an ultrasonic debridement of a phlebostatic ulcer.After LFUD (Figure 2), a patent pending device for Collagenic Infusion Therapy (Genix IT, Italia Medica, Italy) was used (Figure 3). Genix – IT is a collagen device derived from heterologous pericardium and peritoneum in the form of dried sterile and resorbable membranes, 300 - 400 μm thick. The membrane is supported by a drug infusion catheter for bacterial killing and pain control. On its surface the membrane has a few windows of various sizes useful for rapid contact of the infused drugs with the ulcer bed. The same drugs are absorbed by the membrane that transfers them slowly in the ulcer for a prolonged pharmacological action.
 Figure 3. Application of Genix IT on the ulcer bed to promote the formation of granulation tissue; perfusion of the membrane with broad-spectrum antibiotic solution in order to prevent contamination.
Figure 3. Application of Genix IT on the ulcer bed to promote the formation of granulation tissue; perfusion of the membrane with broad-spectrum antibiotic solution in order to prevent contamination.The windows of the collagen membrane also allow drainage of exudate helping to maintain the ulcer clean. Genix IT is placed on the wound bed, fixed to the healthy skin so that the end of catheter is positioned centrally to the upper edge of the lesion and then adapted to its size. The membrane is then irrigated with copious saline and made to adhere to the underlying tissues. Through the catheter, the membrane is then perfused with broad-spectrum antibiotic solution of Ceftriaxone 1g (Figure 3). Perfusion of antibiotic solution will be repeated every 12 hours at home by the patient for 7 days in order to prevent contamination of Genix IT. Perfusion of antibiotic solution was prolonged in all patients who presented clinical signs of local infection of the ulcer (146) until complete remission. The catheter was used in addition to topical analgesic therapy with 2% lidocaine administered by the patient at home following our specific indications, yet for a total of no more than 10 ml per day. Genix IT is completely absorbed after 10-15 days and after that new membranes need to be applied until complete final growth of granulation tissue. The dressing is carried out with the final cover with gauze or in the case of venous insufficiency with zinc oxide compression bandage. The infusion catheter is exteriorized and then firmly fixed (Figure 4).
 Figure 4. Final dressing with zinc oxide compression bandage; the infusion
Figure 4. Final dressing with zinc oxide compression bandage; the infusioncatheter is exteriorized for topical theraphy carried out at home by the patient
EPITHELIAL GROWTH INDUCER
Finalized the growth of granulation tissue, the process of re-epithelialization can often represent a critical phase in the total resolution of the case. With the New Integrated Method we used, for this stage of wound healing, an Epithelial Growth Inducer (Genix EGI) in the form of sterile collagen membranes, 200-250 μm thick, cut into strips 10-12 mm wide, hydrated with copious saline and made to adhere to the edges of the lesion, to allow the re-epithelialization (Figure 5). The Genix EGI is not reabsorbed, left in place for 10-15 days and then removed (Figure 6); an application of new membranes needs to be repeated every 15 days until complete final re-epithelialization (Figure 7 - Figure 8). A saphenectomy was performed in 248 patients after remission of ulcers and antiplatelet and vasoactive therapy was performed in mixed ulcers.
Results
Wound bed preparation is often difficult, painful and frequently protracted for a long time before an ulcerative bed can be treated for stimulate granulation or to perform a dermal implant. Necrotic tissues, fibrina, eschar, as infections prevent tissues growth and that’s why it is preferable to perform their removal in a short time and as radically as possible.
 Figure 5. Finalized the growth of granulation tissue, application of GENIX EGI to the edges of the wound to allow the re-epithelialization.
Figure 5. Finalized the growth of granulation tissue, application of GENIX EGI to the edges of the wound to allow the re-epithelialization.LFUD resulted in this study as well, to effectively solve complex cases of removal of necrotic and very damaged tissues. The effects of fragmentation, emulsification or dissection of LFUD on necrotic or fibrinous material on the bed of ulcer allowed in all treated lesions (312) a radical debridement in a very short time compared to conventional methods, generally done in one sitting. The average time of procedure aimed at obtaining an effective debridement of ulcers using Genera UDD resulted to be 9 sec. per every square centimeter, causing pain less than conventional technique. LFUD was repeated a second time on 32 ulcers in order to improve the implant site of collagen membranes for the presence of formed exudates. The preparation using low doses of lidocaine was sufficient for the execution even of complex debridement. Wound bed preparation with LFUD resulted suitable for accommodate grafts, materials or drugs useful to induce and maintain the granulation process.
 Figure 6. Removal of GENIX EGI after 15 days with complete underlying
Figure 6. Removal of GENIX EGI after 15 days with complete underlyingre-epithelialization.
The possibility of using various types of interchangeable sonic probes with a plastic cover, made it possible to treat ulcers with mixed characteristics according to different densities of adhesion of materials to be removed from ulcer bed, avoiding air and space contamination. Genix IT, placed on the wound bed after ultrasonic debridement, showed the capacity to induce rapid changes in the morphological characteristics of the ulcer. The membrane was completely absorbed after 15 days of implantation resulting to maintain the ulcer bed clean, inducing the gradual reduction of the irregularity of the edges and the appearance of granulation tissue until the complete dermal regeneration. Gradually the intense inflammatory state present around the infected ulcers was attenuated with concomitant reduction in exudation index and rebalancing cellular state. 146 clinically infected ulcers, subjected to local perfusion of antibiotic every 12 hours and prolonged until complete remission, showed a range of time resolution of clinical infection 18-45 days. No single case has shown local or general adverse reactions in antibiotic therapy for the membrane prophylaxis and for the clinically infected ulcers treatment.
 Figure 7. Advanced stage of re-epithelialization after repeated applications of Genix EGI.
Figure 7. Advanced stage of re-epithelialization after repeated applications of Genix EGI.Topical analgesic therapy performed through 2% lidocaine infusion via catheter was very much appreciated by the patients for its efficacy as well as for easy pain management. The time range for pain regression was 4-28 days. In the New Integrated Method, re-epithelialization guided by the means of Genix EGI was effective in terms of rapid healing time of approximately 0.8-1.2cm epithelial growth towards the center of the wound along the entire circumference of the ulcer every 15 days. Genix EGI, unlike GENIX IT, is not reabsorbed, but acts as a substrate for the chemotactic recall of keratinocytes and stimulates and protects epithelial slipping from the periphery towards the center of the wound. LFUD and Collagenic Therapy applied within the New Integrated Method have provided a complete healing of 307 ulcers out of a total of 312. 4 ulcers are in the final phase of healing. 1 ulcer remains unhealed in a patient treated with immunosuppressive drugs anti VEGF.
Discussion
 Figure 8. Final closure of the lesion after 135 days of treatment.
Figure 8. Final closure of the lesion after 135 days of treatment.It has been demonstrated that the re-establishment of a functional ECM is important for the healing of chronic wounds15. It is thus essential to first remove all of the factors that hinder ECM’s formation and immediately after rebalance the cellular activity and accelerate the rate of new tissue formation. LFUD together with Collagenic Therapy integrated in the New Method tackles in synergy all the steps which are necessary to rebalance an altered ECM and to promote dermal and epithelial healing. LFUD has demonstrated to offer significant advantages in wound bed preparation preserving healty tissues during the removal of devitalized tissues, reducing bacterial load and producing biofilm disruption16, characterized by short execution time and minimal pain17. Collagenic Infusion Therapy performed with Genix IT confirmed that by applying collagen ECM to the wound site in form of a membrane, it becomes possible to promote normal progression through the stages of wound healing11. Genix IT, supported by a catheter for drugs infusion, increases the spectrum of therapeutic action regarding the prevention and treatment of infected ulcers and pain control. The use of topical antibiotics still remains controversial18,19,20. However to this date, no studies have been performed using local antibiotic infusion every 12 hours through a catheter for the prevention and treatment of infected ulcers. Our experience with the use of collagen therapy and simultaneous regular infusion of antibiotics produced results that have never been achieved before. However, these results require further verification through culture tests and antibiograms of the changes of bacterial load by the means of Genix infusion Therapy. It is widely recognized and reconfirmed in this study, that topical use of lidocaine significantly reduces pain during and after debridement and has no negative influence on ulcer healing or bacterial flora21. In the New Integrated Method the use of 2% lidocaine resulted to be very effective in the management of ultrasonic debridement and also in the analgesic therapy through a catheter carried out at home by the patients themselves without local or general adverse effects, minimizing the use of systemic analgesics.
Conclusion
LFUD and Collagenic Therapy combined in a new Integrated Method remove the main obstacles in order to rebalance an altered ECM and to promote dermal and epithelial healing. LFUD has proved to be exellent in wound bed preparation for Genix IT implant performed quickly and with minimal pain. Genix IT and Genix EGI guide the dermal regeneration and re-epithelialization and at the same time address the
treatment of infections and pain. The time of clinical resolution of infection using Genix IT was very low even for patients who
previously were found to be unresponsive to prolonged systemic antibiotic therapy. The treatment of underlying diseases and compression therapy with zinc oxide bandages remain essential for the healing of venous leg ulcers, in the New Integrated Method as well.
____________________________
References
1. La Rosa A, Moia R, Ruffoni M, Yusuf M, Blus C, Perversi L, Marone P. Ultrasonic Treatment of Infected Leg Ulcers: Preliminary Results. 15th World Congress of Phlebology of the Union Interna- tionale de Phlebologie - Rio de Janeiro, October 2-7, 2005
2. Serena T, Lee SK, Lam K, Attar P, Meneses P, Ennis W. The impact of noncontact, nonthermal, low-frequency ultrasound on bacterial
counts in experimental and chronic wounds. Ostomy Wound Manage, 2009 Jan; 55(1): 22-30.
3. Risman BV, Rybal’chenko OV, Bondarenko VM, Ryzhankova AV. Repression of bacterial biofilms in suppurative necrotic complications
of diabetic foot syndrome by ultrasound cavitation. Zh Mikrobiol Epidemiol Immunobiol, 2011 Jul-Aug; (4): 14-9.
4. Mendonca DA, Papini R, Price PE. Negativepressure wound therapy: a snapshot of the evidence. Int Wound J 2006; 3:261-271)
5. Medical Advisory Secretariat. Negative pressure wound therapy: an evidence-based analysis. Ontario Health Technology Assessment
Series, 2006; 6(14).
6. Fraccalvieri M, Serra R, Ruka E, Zingarelli E, Antoniotti U, Robbiano F, Viglione M, Frisicale L, Bruschi S. Surgical debridement
with VERSAJET: an analysis of bacteria load of the wound bed pre- and post-treatment and skin graft taken. A preliminary pilot study.
International Wound Journal, April 2011; 8(2): 155–161.
7. Baharestani M. The clinical relevance of debridement. In: Baharestani M, Gottrupp F, Holstein P, Vansheidt W, eds. The Clinical
Relevance of Debridement. Springer-Verlag, Berlin, Heildelberg, New York; 1999:23–80.
8. Nataraj C, Ritter G, Dumas S, Helfer FD, Brunelle J, Sander TW. Extracellular Wound Matrices: Novel Stabilization and Sterilization Method for Collagen-based Biologic Wound Dressings. Disclosures Wounds, 2007; 19(6): 148-156.
9. Loots MA, Lamme EN, Zeegelaar J, Mekkes JR, Bos JD, Middelkoop E. Differences in cellular infiltrate and extracellular matrix of
chronic diabetic and venous ulcers versus acute wounds. J Invest Dermatol, 1998; 111(5): 850-857.
10. Trengove NJ, Stacey MC, MacAuley S, Bennett N, Gibson J, Burslem F, Murphy G, Schultz G. Analysis of the acute and chronic
wound environments: the role of proteases and their inhibitors. Wound Repair Regen, 1999; 7(6): 442 – 452.
11. Cullen B, Watt PW, Lundqvist C, Silcock D, Schmidt RJ, Bogan D, et al. The role of oxidised regenerated cellulose/collagen in chronic wound repair and its potential mechanism of action. Int J Biochem Cell Biol, 2002; 34(12): 1544-56.
12. Ruszczak Z. Effect of collagen matrices on dermal wound healing. Adv Drug Delivery Rev, 2003; 55: 1595–1611.
13. E.A. O’Toole. Extracellular matrix and keratinocyte migration, Black- well Science Ltd Clinical and Experimental Dermatology 2001; 26: 525-530
14. Carville K, et al. Wound Infection in Clinical Practice: An international consensus. International Wound Journal, 2008; 5(supplement 3): 1-11.
15. Loots MA, Lamme EN, Zeegelaar J, Mekkes JR, Bos JD, Middelkoop E. Differences in cellular infiltrate and extracellular matrix of
chronic diabetic and venous ulcers versus acute wounds. J Invest Dermatol, 111(5): 850-857: 1998.
16. Karosi T, Sziklai I, Csomor P. Laryngoscope. Low-frequency ultrasound for biofilm disruption in chronic rhinosinusitis with nasal polyposis: in vitro pilot study. Laryngoscope, 2013; 123: 17–23.
17. Tan J, Abisi S, Smih A, Burnand KG. A painless method of ultrasonically assisted debridement of chronic leg ulcers: A pilot study. European Journal of Vascular and Endovascular Surgery 2006 [Epub ahead of print]
18. Diehr S, Hamp A, Jamieson B. Do topical antibiotics improve wound healing? Journal of Family Practice, February 2007; 56(2): 140-
144.
19. O’Meara S, Al-Kurdi D, Ologun Y, Ovington LG. Antibiotics and antiseptics for venous leg ulcers. Editorial Group: Cochrane Wounds
Group Published Online: 20 JAN 2010.
20. Topical agents or dressings for reducing pain in venous leg ulcers Cochrane Database of Systematic Reviews 2012, Issue 11.
21. Vanscheidt W, Sadjadi Z, Lillieborg S.EMLA anaesthetic cream for sharp leg ulcer debridement: a review of the clinical evidence for analgesic efficacy and tolerability. European Journal of Dermatology, March-April 2001, Synthèse; 11(2): 90-6.
Prof. Antonio La Rosa
Specialista in Chirurgia Vascolare. Chirurgia Sperimentale, Microchirurgia.
Università degli Studi di Pavia
Cell.+39 339/7994760
Tel. +39 0382/24179
www.antoniolarosa.org















